Does My Newborn Have a Tongue Tie?
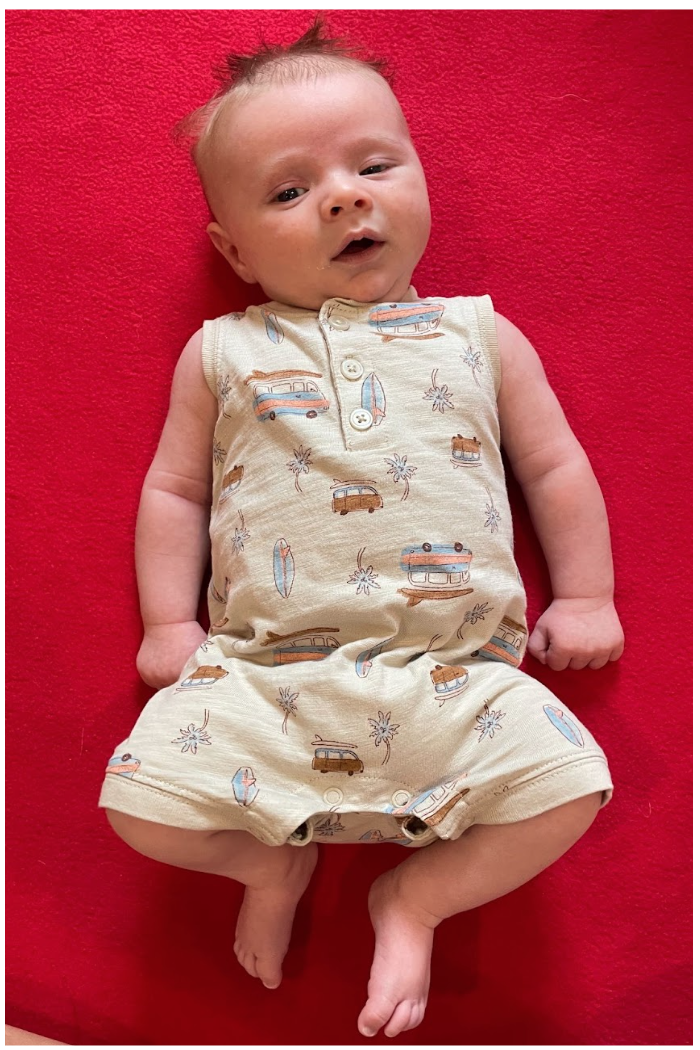
By Dr. Alli Chisholm, PT, DPT
Ah, the tongue tie. Maybe you’ve been told your baby has one, maybe you’ve been told that your baby is fine, and maybe you’ve been told that it would be ridiculous to even consider that your child has a tongue tie that needs to be released.
Being a pediatric physical therapist and a mom, I have seen - and heard - it all. But first, let me to tell you a personal story
When I first became a mom in August of 2021, we had to syringe feed our daughter for the first couple of weeks; she did not effectively breast or bottle feed.
I actually stopped trying to breastfeed after the first few weeks, exclusively pumped and bottle fed, then tried breastfeeding again when my first was around three months old. And I was shocked to find that it worked!
At this time, it’s important to note that I really didn’t know much about ties and no one really mentioned them to me.
Fast forward to my second daughter, and she also had feeding struggles: painful latch for the first week, clicking/smacking noises while feeding, dribbling out of the corners of her mouth, increased spit up, head preference, increased body tension… the works.
I was told by one provider we saw for an evaluation that she had ties and should plan on getting them all released, while my pediatrician told us that her slow down in weight gain had absolutely nothing to do with a tongue tie.
Truthfully, as a mom, I was so lost and stressed out, but with my physical therapist background who has worked with littles with oral restrictions before, I knew there had to be more to the story.
So how do you REALLY know if your little one has a tongue tie? Read on to find out!
What is a Tongue Tie?
Before we can define what a tongue tie is, we first have to talk about what the oral frena are. In the mouth, we all have seven oral frena - two upper cheek, two lower cheek, one upper lip, one bottom lip, and one lingual frenum that can be found under the tongue. Each frenum is a normal tethering of connective tissue in each of these locations that function as a stabilizing factor of the cheeks, lips, and tongue.
A tongue tie is when this connective, stabilizing tissue is actually too tight, causing restrictive movement of the tongue and, in turn, dysfunction of the tongue. This restriction of the lingual - or tongue - frenum is known as ankyloglossia; while oral ties can also be identified as lip or cheek ties, it is most commonly diagnosed that the tissue under the tongue is restrictive, due to the tongue being the biggest contributor to effective breast and bottle feeding. You may have collectively seen oral ties referred to as TOTs, or tethered oral tissue(s).
If a tongue tie is identified, it might be labeled as “anterior” or “posterior”, depending on how far the tethered tissue extends; for instance, if the restrictive tissue extends to the tip of tongue, it may be called an “anterior” tongue tie and - if the tissue is still considered tight but may be visualized further back on the tongue - it might be labeled as a “posterior” tongue tie.
A)Visually, this would be categorized as an anterior tongue tie, which in turn limits tongue mobility, and can be a cause of oral dysfunction. 1.
B) Posterior attachment of the frenum; if this tissue is causing restriction within the mouth and dysfunction as a result, it may be categorized as a posterior tongue tie.
Symptoms of a Tie
Due the restriction that a sublingual tie can cause, below may be symptoms of a tongue tie that can be seen in breastfeeding infants and their mamas2:*
Baby:**
Shallow/ineffective latch
Impaired suckling (to initiate letdown)
Ineffective milk transfer, which could lead to decreased weight gain
Prolonged breast feeding sessions
Decreased satiation after feeds
Chest/breastfeeding parent:
Painful latch
Poor breast drainage
Nipple compression/ damaged nipples
*It is extremely important to note that many breastfeeding dyads with infants who do not have a tongue tie can also experience these symptoms, leading us to the conclusion that a thorough evaluation needs to be completed by a trained professional before diagnosing a tongue tie as being the leading cause of the above symptoms, especially without considering alternate contributing diagnoses.2
**While these symptoms were specifically researched in breastfeeding infants, these symptoms can also be seen in bottle feeding infants with or without a tongue tie, with encouragement to follow the recommendations discussed below if your bottle feeding infant is also experiencing the above symptoms.
Could it be Something Else?
While the evidence on this is limited and/or not supported in the current research, as a clinician treating in this space, I have seen a correlation of babies who present with symptoms of torticollis who have a suspected tongue tie. Torticollis can be defined as a condition where a muscle located in the neck is tight on one side, causing same side bending, or tilting, of the neck and opposite rotation; this can be visualized as a head preference your baby may have to one side or the other.
If there is tightness found in the neck, this can contribute to tightness of the muscles that connect from the hyoid bone - a floating bone located in the front of the neck - up into the jaw, causing tightness in the floor of the mouth and, therefore, mimicking the symptoms of a potential tongue tie.
In addition, if it is observed that your infant will only effectively feed on one breast over the other or while holding in one arm over the other and/or in certain positions, this can also be an indication that there is some sort of restriction in the neck muscles going on versus a true tongue tie.
While it’s possible your little one does indeed have a tongue tie, there is also potential that the restriction in your little one’s mouth is actually neck tightness that, once addressed, may help with the symptoms your little one is experiencing while breast or bottle feeding.
Okay, It Sounds Like My Baby Has A Tongue Tie. Where Do I Go From Here?
If your little one is having difficulty breast or bottle feeding, please know that there is help out there. Find a lactation consultant you trust, as well as a practitioner who can look at your little one using a holistic approach looking at the whole body, like a pediatric physical therapist, occupational therapist, speech therapist, and/or chiropractor.
If a tongue tie is suspected, it is important that you are being seen by a provider who is looking at the whole picture, including taking a thorough medical and lactation history, looking at the baby’s oral anatomical structures, their head and neck positioning, breathing pattern and rate, as well as functional, task-specific issue at hand (ie breast or bottle feeding).1,2
While ENTs, or otolaryngologists, are experienced providers when looking at the head, neck, and airway, their knowledge of infant feeding is limited, so a consultation with a lactation professional is also encouraged.1
Although this blog post is not talking specifically about treatment of oral ties, if a surgical intervention is recommended, I highly encourage seeking out a trusted ENT in your area to look at your little’s airway to ensure that release will not add to or cause obstruction of the airway, or other airway-related issues.
Let’s finish up my story, shall we?
After a lot of contemplation, we did not end up getting a release for the tongue, lip, and potential cheek ties that were originally recommended to us; my mom and PT intuition believed that it would not help our little one’s case.
Does she still have symptoms? At six months old, she does still have some clicking here and there, some spit up, some dribbling, but her weight is perfect for her, her breast and bottle feeding have significantly improved, and she’s the happiest little nugget (as long as she isn’t hungry or tired, that is!).
Once I did my mama/ pediatric PT work with her of looking at her symptoms more holistically, worked on side lying and tummy time, providing manual work as needed, focusing on age-appropriate milestones, and just overall got stronger, she did so much better.
Sources:
Messner AH, Walsh J, Rosenfeld RM, et al. Clinical Consensus Statement: Ankyloglossia in Children. Otolaryngology–Head and Neck Surgery. 2020;162(5):597-611. doi:10.1177/0194599820915457
LeFort Y, Evans A, Livingstone V, Douglas P, Dahlquist N, Donnelly B, Leeper K, Harley E, Lappin S. Academy of Breastfeeding Medicine Position Statement on Ankyloglossia in Breastfeeding Dyads. Breastfeed Med. 2021 Apr;16(4):278-281. doi: 10.1089/bfm.2021.29179.ylf. PMID: 33852342.